Let’s talk about your EHR needs: 1.800.383.6278 MEDHOST Community Login
The core goal of interoperability in the healthcare industry is to help solve a wide range of issues that occur along the care continuum.
By matching patients with their data and improving access through a nationwide healthcare information exchange (HIE), interoperability can have a massive impact in improving population health management. Through broad healthcare interconnectivity, champions of interoperability hope to enhance care quality, empower patients, and help providers become more effective. But what if interoperability could solve for some of the larger issues plaguing healthcare and the nation as a whole, like the opioid epidemic?
Since 1999, the opioid epidemic has claimed 70,200 of American lives. According to a study published by the CDC (Centers for Disease Control and Prevention), in 52 areas in 45 states, opioid overdoses increased by 30 percent from July 2016 to September 2017. The same study also showed that the epidemic is not an isolated rural America problem. In fact, in that same time frame, opioid overdoses in large cities in 16 states increased by 54 percent.
In response to this growing epidemic, the federal government passed a bill named the Substance Use-Disorder Prevention that Promotes Opioid Recovery and Treatment (SUPPORT) for Patients and Communities Act in June of 2018. More recently the CDC and Department of Justice's Bureau of Justice Assistance have incentivized states with grants to help fight opioid abuse by joining a federal backed open-source data sharing hub called RxCheck.
While this type of involvement illustrates the government’s willingness to play a larger role in the fight, according to an article from Politico state support of this mandate is divided at best. Many states have already instituted programs and partnerships with privately held healthcare technology and EHR (electronic health record) vendors as part of a growing movement towards full participation in interoperability—a key to treating the opioid epidemic.
Processes like EPCS (electronic prescribing of controlled substances) create digital trails of prescription medication that have helped increase security, prevent fraud, and provide greater opportunities to hold providers accountable. Conversely, other states have shown that they are already seeing success improving clinical reconciliation and decision support for facilities in their region through privately managed and state-funded interoperability initiatives that often involve state run Prescription Drug Monitoring Programs (PDMPs).
For example, by integrating state-gathered patient medication data with various private facilities’ EHRs, the state of Washington was successful in reducing opioid prescription rates by 25 percent. The state of Wisconsin’s PDMP program, which started in 2015, has led to a 23 percent decrease in monitored prescriptions dispensed. These examples show how effective digitizing the prescriptions process and promoting state-based HIE initiatives can be.
EHR interoperability and its supporting elements can help turn the tide in this epidemic. While many states and private organizations are seeing success, the path toward nationwide interoperability is still complex.
In a letter to the Senate Committee on Finance, the College of Healthcare Information Management Executives (CHIME) outlines various data interoperability barriers to solving opioid issues. They note that consistent identification of opioid abusers and prevention via EHRs, care continuity documentation (CCD), and across state PDMPs continue to present challenges for providers. Based on feedback from clinicians, CHIME state that the extra steps needed to find and record this information on disparate systems breaks-up the clinical workflow.
“A CCD is not necessarily a prescription history,” states MEDHOST Director of Interoperability Brian Laskaris. “Even more so, searching and finding the latest CCD or connecting to a PDMP that can provide the necessary patient information and medication history is challenging enough.”
Laskaris agrees that working out issues to CCD is important; however, he suggests a more targeted solution that focuses solely on medication data may be more effective. While PDMPs stand as a targeted solution that have given providers on a state-by-state basis an advantage, the lack of a secure, standardized process for managing prescriptions across state lines is problematic. In addition to the noted security gaps in the federally sponsored RxCheck solution, patient data and medication access rules differ from state-to-state. In many cases, providers not practicing locally can see but cannot share or save medication histories that may flag habitual abusers.
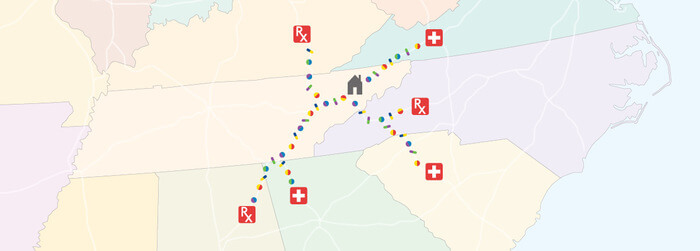
Laskaris gives the example of substance abuse rates in the Johnson City-Bristol, TN-VA area.
The “twin-city” ranks 13 in the top 25 cities for opioid prescription abuse. Its geographic location alone could be one reason abuse rates are so high. Sitting directly on the border of Tennessee and Virginia, the Johnson City-Bristol municipalities are less than 50 miles from West Virginia, North Carolina, and Kentucky. That is five different states an opioid abuser could “shop,” placing prescribing physicians at a disadvantage.
While this is an extreme example on the state-to-state level, this same scenario can easily play out county-to-county or town-to-town.
The CHIME letter notes that thanks to the widespread adoption of EHRs much of the groundwork for leveraging healthcare data technology systems already exists. At the state level, privately held HIEs that integrate PDMPs have shown to generate good results. To get the most out of what is already established and to make marked progress in the battle against opioid abuse further collaboration and standardization are key.
“There are a number of states out there who have shown how participating in interoperability and those types of initiatives can help fight the opioid epidemic,” says Laskaris. “Every effort or partnership has potential. It is good to see that more organizations are making interoperability a priority. As more people find secure ways to share and collaborate, as long as we are allowed to keep building on what has already been shown to work, I am confident we will see the numbers improve.”
The health information technologies and investments needed to turn the tide in this decades-long battle are here, available, and proven to work. If EHR vendors, hospitals, and the government can work together to standardize connections between patient data systems, interoperability can offer serious reinforcements in the fight against opioid abuse.
Learn how we are working to improve care across the entire continuum for a healthier patient population. Email us at inquiries@medhost.com or call 1.800.383.6278.